This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome".
A 62 yr old patient presented to the opd with chief complaints of weakness in the lower limb which makes him unable to walk and move.
He is a farmer by work generally he wakes at 4 and goes to the farm to do his daily work. After that around 7 he returns to home and takes his breakfast. He usually chitchat for some time then he will get back to his field work. He usually sleeps at 8.
History of present illness:
Patient was apparently asymptomatic 5 years back. Then one morning when he woke up he was unable to move his upper and lower limbs. (The night before he was normal doesn't noticed any weakness). He was admitted in Kamineni for about 10 days, he became normal and discharged with some medications prescribed.
After one year he stopped taking medications then he started drinking heavily. After 6 months he experienced another episode of paralysis and admitted in hospital .
He was normal for about 2years and developed 4th attack and admitted here.
Personal history:
Patient takes a mixed diet.
Normal appetite.
Regular bowel and bladder movements.
He was an alcoholic since 30 years and no other addictions.
Past history:
No history of diabetes, hypertension, epilepsy, tuberculosis and asthma.
No allergy to known drugs.
Family history:
No such relevant history is seen in the family.
General examination:
Patient was cooperative, coherent, conscious and well oriented to the surroundings.
No pallor.
No icterus.
No clubbing.
No generalized lymphadenopathy.
No cyanosis.
No bilateral pedal oedema.
Vitals:
Pulse rate-90bpm
Blood pressure- 110/80mm of hg
Respiratory rate-20 per min.
Spo2-98%
Systemic examination:
Cardiovascular system-
Chest wall is bilateral symmetry.
No visible pulsations.
JVP is normal.
S1 and S2 are heard.
Respiratory system-
Bilateral airway.
Trachea is in midline.
No added sounds.
Per abdominal
Abdomen is soft and tender.
Bowel sounds are heard.
No palpable mass or free fluid.
Central nervous system -
Reflexes-
B - -
T - -
S. - -
K. +1 +1
A. -. -
Plantar - flexor Flexor
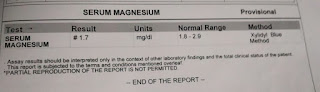
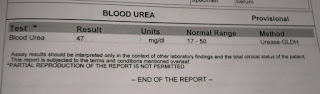
Investigations:
PROVISIONAL DIAGNOSIS
? HYPOKALEMIC PERIODIC PARALYSIS
PLAN OF TREATMENT
1. Inj. Kcl 2 amp in 500ml Ns over 4.5 hours
2. Inj. Thiamine 1 amp in 100 ml NS iv tid
3. Syp. Potachlor 10 ml po TID
4. Inj.pan 40 mg iv OD bbf
5. IVF 1 NS , 1RL @ 100 ml/hr
6. Tab.dolo 650 mg po sos
25/10/21
SOAP NOTES DAY 3
AMC bed 2
S:
C/O muscle aches
Weakness improved
O:
Patient is conscious coherent and cooperative
Temp: 98.6 F
BP: 110/80 mmHg
RR:18CPM
PR:80BPM
CVS: S1,S2 heard
RS: NVBS+,no crepts
P/A: soft ,non tender
GRBS:110 mg/dl
I/O :2600/2100
SPO2:98%
A:
? HYPOKALEMIC PERIODIC PARALYSIS
P:
1)inj thiamine 1 amp in 100 ml NS iv Tid
2)inj.kcl 2 amp in 500 ml NS iv over 4-5 hrs
3)inj.pantop 40 mg IV OD BBF
4)Tab.Dolo 650 mg po sos
5)syp.potchlor 15 ml po Tid
6) continuous ECG monitoring
26/10/21
SOAP NOTES DAY 4
AMC bed 2
S:
C/O Tingling in the hands and feet, weakness improved
O:
Patient is conscious coherent and cooperative
Temp: 98.6 F
BP: 110/80 mmHg
RR:18CPM
PR:80BPM
CVS: S1,S2 heard
RS: NVBS+,no crepts
P/A: soft ,non tender
GRBS:110 mg/dl
I/O :2600/2100
SPO2:98%
A:
? HYPOKALEMIC PERIODIC PARALYSIS
P:
1)inj thiamine 1 amp in 100 ml NS iv Tid
2)inj.kcl 2 amp in 500 ml NS iv over 4-5 hrs
3)inj.pantop 40 mg IV OD BBF
4)Tab.Dolo 650 mg po sos
5)syp.potchlor 15 ml po Tid
6) continuous ECG monitoring
27/10/21
SOAP NOTES DAY 5
AMC bed 2
S:
No present complaints
O:
Patient is conscious coherent and cooperative
Temp: 98.6 F
BP: 110/80 mmHg
RR:18CPM
PR:80BPM
CVS: S1,S2 heard
RS: NVBS+,no crepts
P/A: soft ,non tender
GRBS:110 mg/dl
I/O :2600/2100
SPO2:98%
A:
? HYPOKALEMIC PERIODIC PARALYSIS
P:
1)inj thiamine 1 amp in 100 ml NS iv Tid
2)inj.kcl 2 amp in 500 ml NS iv over 4-5 hrs
3)syp.potchlor 15 ml po Tid
4) continuous ECG monitoring












Comments
Post a Comment