Case 3
"This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome".
A 30 year old female patient came to the casuality with cough since 20 days and shortness of breath since 4 days back.
History of present illness:
-Patient was apparently asymptomatic 20 days back and the cough is insidious on onset and intermittent and associated with expectoration which is whitish in colour .
-Cough is associated with fever which is low grade and intermittent.
-And also associated with rightsided chest pain which is sharp pricking type.
-Patients complains of shortness of breath since 4 days and is of non progressive.
History of past illness:
-No similar complaints in the past.
-There is no history of diabetes, hypertension, asthma, tuberculosis and epilepsy.
Personal history:
Diet- Mixed.
Apetite - Normal.
Sleep-adequate.
Bowel and bladder movements - Regular.
Addictions -No.
Family history:
No history of such complaints in the family.
General examination:
Patient is cooperative, coherent and conscious.
He is well oriented to time, place and person.
-Physical examination-
No pallor.
No ecterus.
No cyanosis .
No clubbing .
No generalised lympadenopathy and
No oedema.
Vitals-
Blood pressure-130/70mm of hg.
Pulse pressure-72/min
Respiratory rate-18/ min
Spo2-96% at room air.
-Systemic examination:
Circulatory system-
Chest wall is bilateral symmetrical.
No visible pulsations, engorged veins, scars.
Respiratory system-
Dysapnea is present.
Having inspiratory crepts and wheeze.
Position of trachea is central.
Breathe sounds are vesicular.
Adventitous sounds rhonchi and rales.
Per abdominal
Abdomen is smooth and nontender.
Bowel movements are heard.
No palpable mass or free fluid.
Auscultation:
S1 and S2 are heard.
Central nervous system:
Patients is conscious.
Speech is normal.
Reflections are normal.
Provisional diagnosis:
Viral pneumonia
Investigations:
Hemogram
Heamoglobin-11. 5
Total leucocyte count-12500
PLT-4. 9
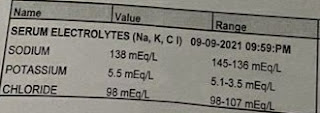
Serum Electrolytes:
Treatment Given
On Day 1:
1.IVF-2 NS @75ML/HR
2.INJ OPTINEURON 1 AMP IN 100 ML NS IV OD
3.SYP ASCORIL 10 ML PO BD
4.TAB AUGMENTIN 625 MG PO BD
5.TAB PCM 650 MG PO BD
6.TAB PAN 40 MG PO OD
7.NEB WITH BUDECORT 12 TH HRLY,DUOLIN 8TH HRLY
8.MONITOR VITALS 4TH HRLY
DAY 2:
1.IVF-RL, NS @75ML/HR
2.SYP ASCORIL 10 ML PO BD
3.TAB AUGMENTIN 625 MG PO BD
4.TAB PCM 650 MG PO BD
5.TAB PAN 40 MG PO OD
6.NEB WITH BUDECORT 12 TH HRLY,DUOLIN 8TH HRLY
7.TAB AZITHRAL 500 MG PO OD
8.INFORM SOS
DAY 3:
1.IVF-RL, NS @75ML/HR
2.SYP ASCORIL 10 ML PO BD
3.TAB AUGMENTIN 625 MG PO BD
4.TAB PCM 650 MG PO BD
5.TAB PAN 40 MG PO OD
6.NEB WITH BUDECORT 12 TH HRLY,DUOLIN 8TH HRLY
7.TAB AZITHRAL 500 MG PO OD
8.INFORM SOS
Advice at Discharge
1.TAB AUGMENTIN 625 MG PO BD FOR 3 DAYS
2.TAB PAN 40 MG PO OD FOR 5 DAYS
3.SYP ASCORIL 10 ML PO BD
4.TAB PCM 650 MG PO BD FOR 5 DAYS




Comments
Post a Comment